What is knee cartilage damage?
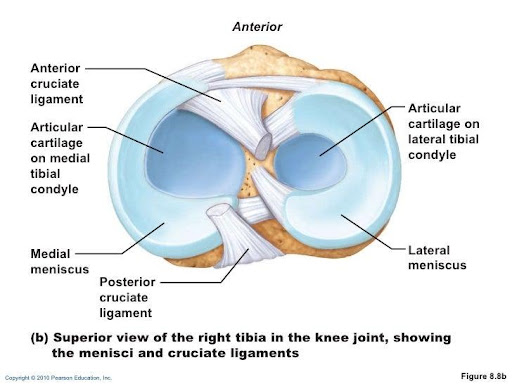
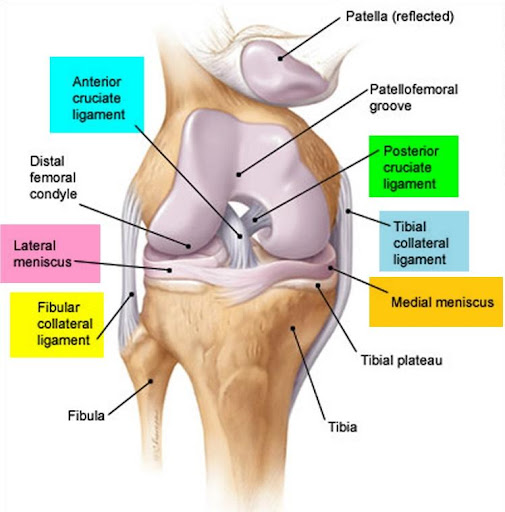
The Knee joint is sandwiched between the bottom of thigh bone (femur) and top of shin bone (tibia). Cartilage is akin to a thin layer of grout attached to ends of femur and tibia to facilitate smooth motion between these two bones which allows the knee joint to bend and straighten. It acts as a lubricant between the joint surfaces. The C-shaped structures (often called meniscal cartilage or simply meniscus) function as shock absorbers and help to spread the body weight evenly among the cartilage (see pictures below). Ligaments are ribbons of varying elasticity which help maintain the stability of the knee.
Cartilage damage can occur following a blow, recurrent minor traumas, or due to a growth imperfection. The damaged cartilage comes away from its natural position alone or with a small piece of underlying bone. It can come away partially creating a flap, or completely leaving a fragment that can move around the joint. The area of damaged cartilage can vary in size and depth. Ligament or meniscal damage can be associated with these injuries.
What happens when a cartilage is damaged?
Articular cartilage does not have blood supply therefore, when it gets damaged, it is very difficult for the damage to heal. Further, this damaged part can break down into the joint causing symptoms. This damaged part can catch on other structures causing locking of the knee with difficulty in moving the knee joint. When your surgeon suspects a cartilage damage, he usually orders an MRI scan which is specifically suited to detect cartilage, meniscal and ligamentous injuries. Surgery will be proposed in the case of a symptomatic flap or fragment, or a major cartilage defect. The objective of the operation is to restore a uniform sliding surface to relieve the pain, locking and swelling, and enable a return to normal walking and activities, thus preventing the progressive deterioration of the joint.
What is cartilage surgery?
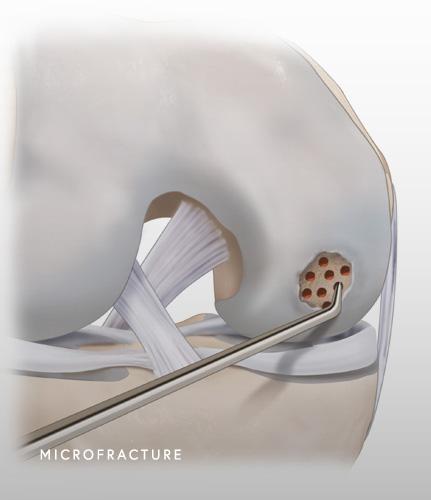
Cartilage surgery is a procedure where the surgery aims to stimulate cartilage repair or replace the damaged cartilage. Cartilage stimulation and repair is good only for smaller lesions. It is called microfracture where the lesion is deepened, and multiple punctures are created into the cartilage (see image below) until bleeding occurs and healing is stimulated by release of growth factors from bone marrow.
When the damage is more extensive and covers a large surface area, then microfracture is less successful. This extensive damage is usually treated by removing the damaged cartilage and replacing it with cartilage (osteochondral graft) from another part of the knee cartilage (usually non weight bearing cartilaginous part of the knee). It is also called mosaicplasty. The aim of this treatment is to create a homogenous sliding surface.
Cartilage surgery is usually performed by keyhole surgery (arthroscopy) where two small cuts are made in front of the knee. The arthroscope (camera) is inserted through of these cuts to investigate the joint. The knee joint is distended with saline to facilitate the move of the instruments inside the joint and thereby avoid any iatrogenic damage to the cartilage by the surgical instruments. Small instruments are inserted through the other incision to carry out the surgery. The operation lasts about half an hour, and it is usually done as a day case procedure where the patient can go home the same day.
The operation is carried out under regional or general anaesthesia. Your anaesthesiologist will decide with you the best type of anaesthesia according to your state of health. After the operation, the incisions are covered with a sterile dressing, which is left in place for 10 days. The pain will be managed and monitored very closely during the post-operative period, and the treatment will be adjusted accordingly.
Post-operative rehabilitation and return to activities
Rehabilitation starts with physiotherapy after the surgery. The main objective is to get the knee moving and getting back the strength in the muscles. Depending on the type of cartilage surgery, you may have to mobilise with crutches with restricted weight bearing status. Driving and returning to work is usually around 6-8 weeks depending on the profession. Gentle sporting activity such as cycling, and swimming can be resumed after 3 months. Full return to sporting activities can take as long as 6 months.
What are the risks and complications?
In addition to the risks associated with any surgery and the anaesthetic, there are some risks specific to this surgery: (this list is not exhaustive)
- Bleeding inside the joint leading to hematoma. If it is small, it can be left alone, however if it is big, then it might have to be drained
- Knee stiffness, especially if the physiotherapy regimen is not strictly adhered to.
- The occurrence of an infection, although rare (risk below 1 %), is a serious complication and may require surgical revision and a course of antibiotics.
- Blood clots in legs (DVT-Deep Vein Thrombosis) and lungs (PE- Pulmonary Embolism) can occur, especially in high-risk patients such as those with previous history of DVT/PE, family history and history of cancer. It is essential that you pass on this information to the surgical team before the surgery. If you develop this complication, you will be put on anticoagulants to thin the blood.
- The mobilisation of a graft or the displacement of a fixed cartilage fragment can occur and require revision surgery.
What is the expected outcome of the operation?
Whichever procedure is performed, the locking, swelling and instability will disappear rapidly after the operation. The healing rate of cartilage surgery varies depending on the type of cartilage surgery performed. Regarding the microfracture technique, the improvement in cartilage function and condition is about 80 % in the case of an isolated cartilage lesion. Regarding mosaicplasty, moderate discomfort around the harvesting site is observed in about 15 % of cases. Nevertheless, the results remain very encouraging as good results are obtained in most of the cases
